
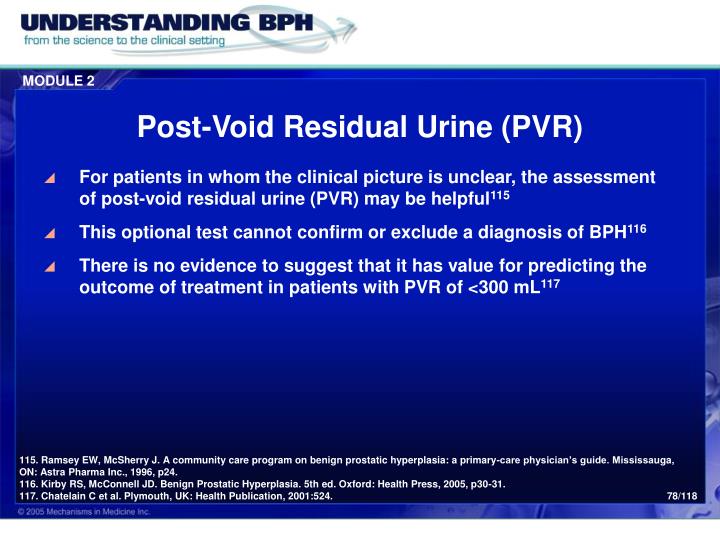
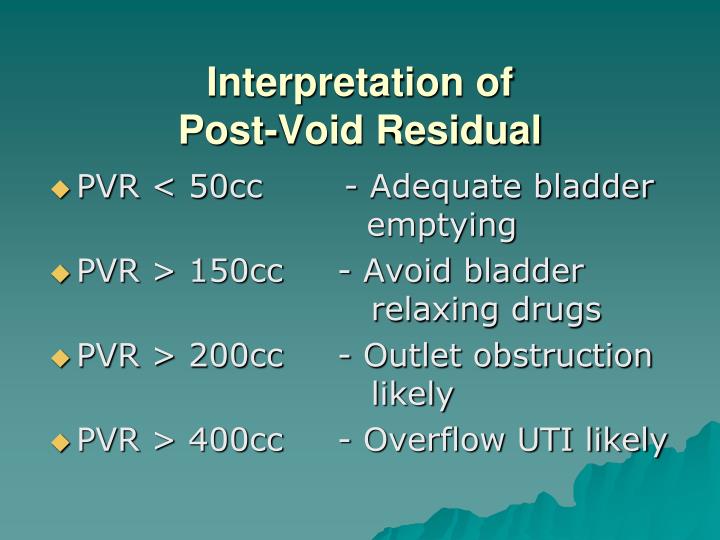
Following chart review, we identified 266 women with pre-operative urodynamics followed by prolapse repair. Urodynamics were performed by multiple providers according to their standard practice prior to surgical repair of prolapse. A two-reviewer case-by-case retrospective chart review of each medical record was performed on the 358 patients and data extracted into REDCap 9 for: demographics urodynamic parameters re-review of urodynamic tracings pre-operative prolapse stage date of surgery type of surgery the date and volume of all post void residuals (PVR) after surgery. Our bioinformatics data core exported demographic codes, International Classification of Disease codes (ICD-9 & ICD-10), and additional CPT billing codes. We then identified 358 records from this group with possible pre-operative urodynamic CPT codes. We sought to describe outcomes associated with the large capacity bladder in women who subsequently underwent anterior and/or apical prolapse repair at our institution over a 6-year period.Īfter obtaining institutional review board approval, we identified 592 sequential patient records, which contained anterior and/or apical prolapse repair Current Procedural Terminology (CPT) codes at our single institution from 2009 to 2015. Given the lack of quantification of bladder capacity by traditional nomograms, improvements in post-void residual and voiding efficiency following prolapse repair in patients with a large capacity bladder have been poorly defined. Voiding efficiency is a measure of voided volume expressed as a percentage of bladder capacity. What is not defined by these nomograms is the influence of large bladder capacity on voiding efficiency in the setting of pelvic organ prolapse. However additional nomograms have identified much lower pressure cutpoints (20–25cmH2O) than Blaivas and Groutz, 4 and have included the addition of flow cutpoints (11–15mL/s) and fluoroscopic criteria (Chassagne, 5 Nitti, 6 Lemack and Zimmern, 7 Defreitas 8). The most commonly cited female obstruction nomogram was published by Blaivas and Groutz, 4 which classified women into three grades of obstruction, based on the voiding detrusor pressure cutpoints of 57 and 107cmH2O for differentiating mild, moderate and severe obstruction. As such, urodynamic pressure flow evaluation has been a standard for ascertaining a patient’s likelihood of spontaneous void following prolapse repair.
Cpt code for post void residual bladder scan driver#
Since bladder symptoms are a considerable driver of patient’s decision to pursue prolapse repair, and incomplete bladder emptying is one of the most common lower urinary tract dysfunctions encountered in these patients, pre-operative expectations are a major driver of a patient’s perception of a successful surgical outcome. 2 Surgical correction of anterior and/or apical prolapse results in anatomic unkinking of the bladder outlet by realigning the bladder with the bladder neck and urethra, which in theory corrects anatomic outlet obstruction. 1 Incomplete bladder emptying can be caused by a weak bladder and/or bladder outlet obstruction. Pelvic organ prolapse can result in kinking of the bladder neck and bladder outlet obstruction.


 0 kommentar(er)
0 kommentar(er)
